BMI Isn’t the Whole Story
BMI Isn’t a One-Size-Fits-All Health Measure — So How Should We Really Use It?
Most people have heard of Body Mass Index, or BMI. Many even know their number. What’s less commonly discussed is how this simple calculation became such a powerful tool in healthcare — and why it increasingly fails to reflect real health risks for large sections of the population, especially in India and other South Asian countries.
BMI was never meant to define individual health. Yet today, it often determines who gets medical advice, who qualifies for treatment programmes, and who is considered “at risk.”
Where BMI Came From — and What It Actually Measures
BMI was developed in the 19th century using data from a narrow population group. It calculates health risk by dividing weight by height squared. The method was designed to study population trends, not to assess individual bodies.
What BMI really measures is body size, not body composition.
It does not distinguish between:
Fat and muscle
Visceral fat and subcutaneous fat
Bone density differences
Ethnic and genetic variations
A muscular person may be labelled overweight, while someone with high body fat but low muscle may fall within a “normal” range.
Why BMI Misses the Mark for Indians and South Asians
In India, the limitations of BMI become even more obvious. Research over the years has shown that South Asian populations tend to:
Develop diabetes and heart disease at lower BMI levels
Accumulate more abdominal and visceral fat
Experience metabolic risk even when not visibly overweight
This means that many Indians face serious health risks while still falling within what BMI defines as a “healthy” range.
As a result, conditions like:
Type 2 diabetes
Fatty liver disease
Hypertension
Heart disease
often go undetected until they are well established.
The Problem With Universal BMI Cut-Offs
Global BMI thresholds assume that health risks rise uniformly across populations. In reality, they don’t.
For many Indians, metabolic risk begins at BMI levels that are still considered acceptable by international standards. When doctors rely too heavily on BMI alone:
Early warning signs are missed
Preventive screenings are delayed
Lifestyle interventions are not offered in time
This creates a gap where large numbers of people appear “low risk” on paper but are actually vulnerable.
Why BMI Still Persists in Healthcare
Despite its flaws, BMI continues to be widely used because it is:
Easy to calculate
Inexpensive
Consistent across large populations
Useful for broad public health monitoring
For population-level trends, BMI still has value. The problem arises when it becomes the sole indicator of individual health.
What Should Replace or Support BMI?
Rather than abandoning BMI altogether, many healthcare professionals now see it as just one piece of a much larger health picture.
Better assessments often include:
Waist circumference
Waist-to-hip ratio
Blood sugar levels
Cholesterol profile
Blood pressure
Physical activity levels
Diet patterns
Family history
In many cases, waist circumference has proven to be a stronger indicator of metabolic risk than BMI alone — especially for Indian patients.
Why This Matters for Preventive Healthcare in India
India is facing a rapid rise in lifestyle-related conditions. Early identification of risk is critical.
When BMI thresholds are treated as fixed rules:
People miss out on early counselling
Screening tests are postponed
Preventive care becomes reactive instead of proactive
A more flexible, individual-focused approach allows doctors to intervene before disease sets in.
The Role of Specialised Medical Departments
Managing weight-related and metabolic health requires a multidisciplinary approach, involving:
Endocrinology for diabetes and hormonal balance
Internal Medicine for overall metabolic assessment
Cardiology for heart health
Nutrition and Dietetics for personalised dietary planning
Preventive Medicine for early risk management
On TheThs.com, users can easily find and compare doctors, hospitals, clinics, and wellness centres across these specialties.
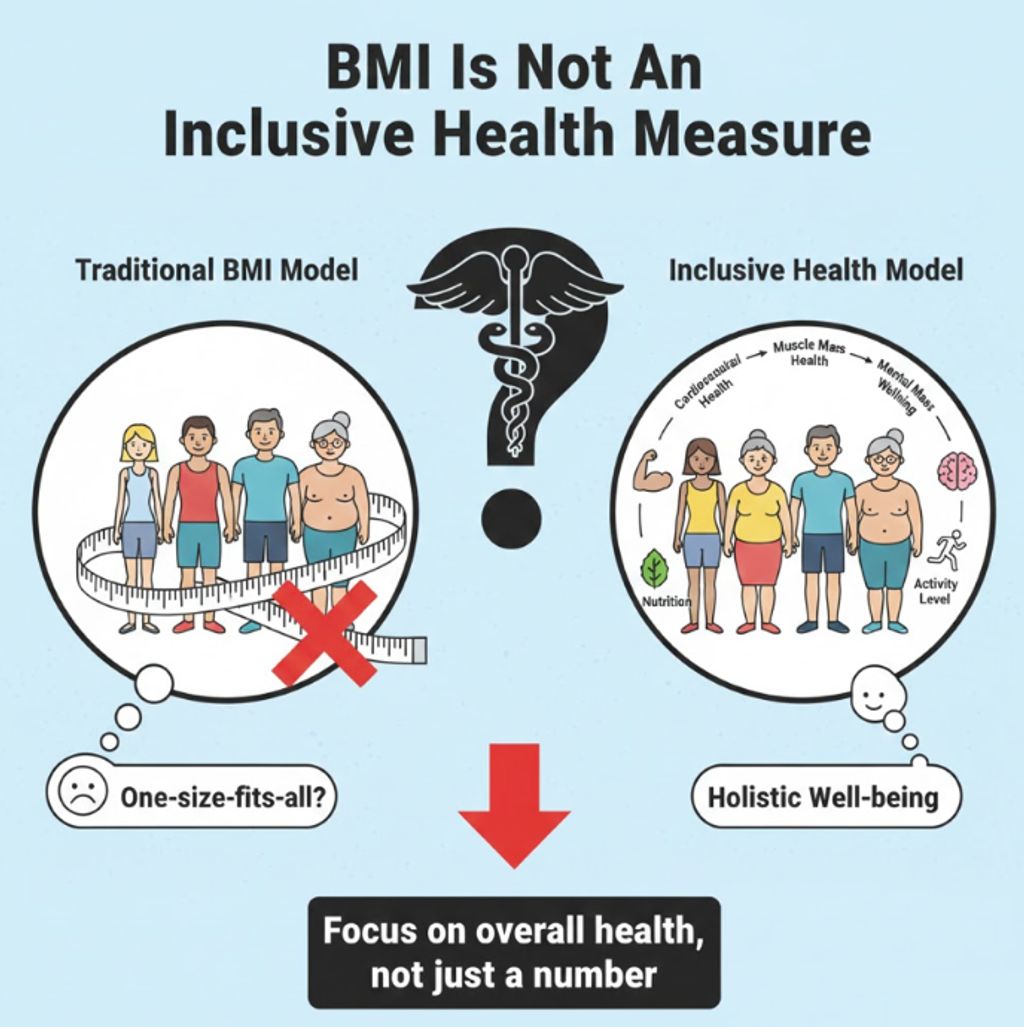
Moving Toward More Inclusive Health Metrics
Health is not a number — it’s a combination of biology, lifestyle, environment, and access to care. While BMI may remain part of medical conversations for now, its role is gradually changing.
The future of healthcare lies in:
Personalised risk assessment
Culturally relevant guidelines
Early, inclusive screening
Holistic evaluation beyond weight alone
Conclusion
BMI was never designed to define individual health — and for populations like Indians, relying on it too heavily can be misleading. Used carefully, it can still offer insight. Used alone, it can hide risk.
A more complete picture comes from combining BMI with other clinical markers, lifestyle factors, and medical evaluation. Platforms like TheThs.com help bridge this gap by connecting individuals to the right specialists, diagnostics, and preventive care — enabling health decisions that go beyond a single number.